You’re just stressed, right?
We all go through periods of stress in our lives. It usually ebbs and flows, but often has a distinct start and stop points. Getting into college, graduating college, grad school, engagement, wedding, new jobs, pregnancy, infancy, toddlerhood, teenagers, work, empty-nest, retirement, illness, loss of a parent, etc. Those all sound pretty familiar to a lot of people.
Then every once in a while something happens that just smacks you in the face and seems like there isn’t an end in sight. Maybe that’s a marriage that’s lacking happiness or a job that doesn’t have meaning. Those experiences seem hard to overcome. Or one day a traumatic event reminds you of something that happened as a child and emotions come pouring back out. Or a motor vehicle accident sends you into a tailspin of brain fog, confusion, fatigue, and pain that you can’t imagine how you will ever escape.
What all of these events have in common is stress. The stress response is a uniquely homogenous experience, one that affects all people: man, woman, child, elderly, adolescent. It is not spared in any one person and it is centrally mediated, meaning the brain and spinal cord play a tremendous role. We all have different strengths as it comes to dealing with stress, whether that be due to coping strategies or differing thresholds, but what none of us control is the unconscious physiologic events that occur when something we experience is perceived by the brain as stressful.
To understand this a bit more and to learn why stress is so deleterious for our long-term health, we need to get into the weeds a bit to really understand the physiologic event that triggers stress and the events that keep it going.
The Nervous System
Our Central Nervous System (CNS) is the grand central station for all processes in our body. It is comprised of our spinal cord and brain. The job of the CNS is to interpret information from the periphery and coordinate the responses. The brain is the most complex organ we have and is made up of four regions: the temporal lobe, parietal lobe, frontal lobe, and occipital lobe.
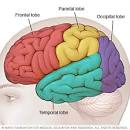
Here’s a breakdown of each of the lobes:
Temporal lobe (green): important for processing sensory input and assigning it emotional meaning. It is also involved in laying down long-term memories. Some aspects of language perception are also housed here.
Occipital lobe (purple): visual processing region of the brain, housing the visual cortex.
Parietal lobe (yellow): the parietal lobe integrates sensory information including touch, spatial awareness, and navigation. Touch stimulation from the skin is ultimately sent to the parietal lobe. It also plays a part in language processing.
Frontal lobe (pink): positioned at the front of the brain, the frontal lobe contains the majority of dopamine-sensitive neurons and is involved in attention, reward, short-term memory, motivation, and planning.
The spinal cord is responsible for carrying information to and from the brain and the periphery. Think of the spinal cord as the mailman. It is full of circuits that control certain responses, reflexively, as well as control of muscle groups. The brain provides the input but the spinal cord does the work.
The Peripheral Nervous System (PNS) is a system of nerves that connect the CNS to every other structure. It has two subdivisions: the somatic and autonomic nervous systems. The somatic system is responsible for voluntary motor control of skeletal muscle and is comprised of cranial and spinal nerves. The autonomic is further subdivided into parasympathetic and sympathetic nervous systems, both of which are involuntarily controlled as well as the enteric system which controls the gastrointestinal system and also functions involuntarily. The enteric nervous system is often considered the “second brain” and has been thoroughly investigated by researchers for decades, including Dr. Michael Gershon, who has been able to link the pit we get in our guts to experiences of anxiety or fear. We talk more about this relationship in an earlier post that describes how our gut and brain are interconnected. Read most about that here.
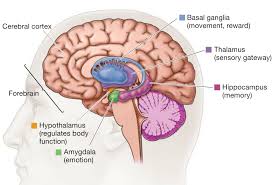
Let’s talk more about the Autonomic Nervous System (ANS)
The ANS (a division of the PNS) is responsible for the innervation of smooth muscle and glands and is often referred to as the vegetative system as it controls most of our organs without any voluntary control. Acting largely unconsciously, it controls our heart rate, respiration rate, digestion, pupillary response, urination, and sexual arousal. It is located inside the brain and is heavily regulated by the hypothalamus. Functions regulated by the ANS include control of respiration, cardiac regulation (the cardiac control center), vasomotor activity (the vasomotor center), and certain reflex actions such as coughing, sneezing, swallowing, and vomiting. The hypothalamus, located just above the brain stem, behaves as an integrator for autonomic functions, receiving ANS regulatory input from the limbic system to do so.
The Sympathetic Nervous System
Frequently referred to as our “fight or flight,” this system is responsible for coordinating behaviors that would allow us to flee danger. More accurately, it is responsible for the up and downregulation of hormonal and neuronal stress responses. It is constantly working to maintain the homeostasis of our hemodynamics (basically put, it is making sure we have enough blood where we need it). This system operates by releasing acetylcholine (a neurotransmitter) which subsequently results in the release of norepinephrine (hormone and neurotransmitter). The release of norepinephrine activates the adrenergic receptors that are present in the tissues in the periphery thus triggering a state of readiness.
The sympathetic nerve ganglia (home base of the cells) originate from the center of the spinal cord located in the thoracic spine starting at T1 and are thought to extend to the second or third lumbar vertebrae. This is an important concept to note, as the SNS is thought to have to “thoracolumbar outflow” which plays a role in the treatment of chronic sympathetic tone.
The adrenal medulla (which is part of the adrenal gland and is largely responsible for hormone production that regulates both metabolism and the immune system) produces epinephrine (adrenaline), norepinephrine (noradrenaline), and a small amount of dopamine in response to stimulation by sympathetic neurons. The relationship between the adrenal gland and the sympathetic nervous system is necessary to draw because this relationship is often the cause of adrenal fatigue, which we will further explore below.
All of the mechanisms described above are meant to prime the body for action.
The Parasympathetic Nervous System
The “rest and digest” system, the parasympathetic nervous system is responsible for activities within the body while at rest. Beginning in the ganglia of the central nervous system, the parasympathetic nerves arise from three specific areas:
- The Cranial Nerves III, VII, and IX
- The Vagus Nerve
- The Splanchnic Nerves
The cranial nerve origin of the parasympathetic nervous system is responsible for eye, mouth, and nasal regulation whereas the pelvic-splanchnic parasympathetic nerve fibers are responsible for pelvic visceral innervation. The visceral tissues in the pelvis that the parasympathetic nerve pathway controls include those of the urinary bladder, ureters, urinary sphincter, anal sphincter, uterus, prostate, glands, vagina, and penis. Through unconscious measures, the parasympathetic system will cause peristaltic movements of the ureters and intestines, move urine from the kidneys into the bladder and food down the intestinal tract, and, upon necessity, the parasympathetic will assist in excreting urine from the bladder or defecation. Activation of the parasympathetic will cause the detrusor muscle (urinary bladder wall) to contract and simultaneously relax the internal sphincter muscle between the bladder and the urethra, thus allowing voiding of the bladder. Defecation occurs by means of parasympathetic stimulation of the internal anal sphincter yielding total relaxation. There are other skeletal muscles involved with these processes but the parasympathetic plays a huge role in continence and bowel retention. The vagus nerve serves primarily to regulate the cardiac and pulmonary tissue, larynx, and tracheal tissue.
So what happens when we’re in a prolonged state of stress?
The amygdala, or our emotional processing center, sends distress signals to the hypothalamus. The hypothalamus functions as the commander, working through the ANS to coordinate the appropriate response (either prep the body to go or slow the body to rest). In response to a distress signal, the SNS stimulates the adrenal gland to start pumping adrenaline (epinephrine) and other stress hormones into the bloodstream. As the adrenaline spreads through the body, we see several physiologic events occur: an increase in heart rate, blood pressure, and respiration. All these events occur to deliver blood to organs and tissues and increase oxygenation through small airways. This increases alertness to the brain improving its perception of the environment. Epinephrine also triggers the release of glucose (blood sugar) and fats from temporary storage sites throughout the body. Interestingly enough, all of this happens before the person is even visually aware of said stressors.
Watch this 2-minute neuroscience video on the amygdala
Once this initial surge of epinephrine calms down, the body releases a second response system, called the HPA axis. This response system consists of the hypothalamus, the pituitary gland, and the adrenal gland. The HPA axis relies on input from a variety of hormonal shifts to keep our body in the “go” mode. If the brain continues to detect danger, the hypothalamus releases corticotropin-releasing hormone (CRH), which talks to the pituitary gland, triggering the release of adrenocorticotropic hormone (ACTH). This hormone travels to the adrenal glands, prompting them to release cortisol. The body thus stays revved up and on high alert. When the threat passes, cortisol levels fall. The parasympathetic nervous system — the “brake” — then dampens the stress response.
Central Sensitization
Unfortunately, there are times when the body continues to perceive threat even though the event has ended which keeps the HPA axis activated. Persistent epinephrine surges can damage blood vessels and arteries. Elevated cortisol levels create physiological changes that help to replenish the body’s energy stores that are depleted during the stress response which inadvertently contribute to the buildup of fat tissue and to weight gain in an effort to store more energy.
In this heightened state, the body over-produces adrenaline and cortisol and ultimately wears out the adrenal gland which eventually becomes depleted. Ultimately, the thyroid gland becomes taxed as well, contributing to increased feelings of fatigue and depression. According to Smith and Vale, the emotional and memory system of the brain, known as the limbic system, play a key role in slowing down HPA axis. Unfortunately, for people who have experienced significant trauma, including relentless pain and/or failed treatment, the amygdala is hyperactivated causing increase activation of HPA axis thus resulting in delayed activation of the parasympathetic nervous system.
Central sensitization is the theory that prolonged stimulation/input causes increased perception and output, meaning that it takes less input to cause the same if not more output. Essentially, our threshold for stress is lowered and our response is enhanced meaning that our fight-or-flight is activated at much lower levels than have previously been activated and thus the response system stays “on” for longer periods of time. Easily put, it takes less of a “stress” to cause more of a response.
What does that mean for me, I don’t have that much stress?
Generally speaking, most people don’t fully appreciate the plethora of occasions in which the body interprets an event as stress. It doesn’t always have to look like stress to be stressful.
Here is a list of common causes of prolonged stress:
- Anger
- Fear / Worry /Anxiety
- Depression
- Guilt
- Overwork/ physical or mental strain
- Excessive exercise
- Sleep deprivation
- Light-cycle disruption
- Going to sleep late
- Surgery
- Trauma/injury
- Chronic inflammation
- Chronic infection
- Chronic pain
- Temperature extremes
- Toxic exposure
- Malabsorption
- Maldigestion
- Chronic illness
- Chronic-severe allergies
- Hypoglycemia
- Nutritional deficiencies
All that said, you may just be in a heightened state of fight or flight and not even know it. But that would likely explain your inability to get rid of those few extra pounds, or dry skin or nagging headache. Finding professionals who understand these processes will be paramount in overcoming whatever problem you may be dealing with.
Is there anything I can do about this myself?
We know that stress management techniques are imperative and working with a behavioral health therapist will help work through which techniques are best for you but you could also use trial and error. Journaling, meditation, deep breathing, and visualization are all great options that are well supported by research. Mindfulness practice performed regularly has been shown to decrease the size of the amygdala thus lessening the likelihood of excessive HPA axis activation.
Exercise is also a good tool to use to restore homeostasis however too much exercise can have the opposite effect. There is a fine line to walk which just requires practice to see how your body responds to certain dosages of exercise. Additionally, choosing the right exercise for your body is equally important.
Eating regular meals is helpful as it keeps a steady blood sugar level which allows the adrenals to not be over-taxed. Keeping good blood sugar levels will also allow for a clear head and reduce cravings, anxiety, and fatigue. Avoiding caffeine, alcohol, and processed foods which all contribute to dehydration.
There is evidence to suggest the use of supplementation when in chronic adrenal fatigue but that should be addressed with your physician or registered dietitian to address your specific needs.
____________________________________________
About the author:
Dr. Sarah Cash Crawford, PT, DPT, COMT, CMTPT, is a physical therapist and certified myofasical trigger point therapist through Myopain Seminars ®, the only certifying body of Trigger Point Dry Needling in the US. Dr. Crawford trained under Jan Dommerholt, PT and founder of Myopain Seminars ®, who worked directly under Drs. Travell and Simmons in his pursuit to bring dry needling to the U.S. Dr. Crawford has been performing Trigger Point Dry Needling in the Cincinnati area for over six years and was the first CMTPT in the state of Ohio. She has been practicing physical therapy for eight years. With a background in neurologic rehabilitation, manual therapy, and a specialty in treating chronic pain, Dr. Crawford began studying dry needling to further expand her treatment options to help patients overcome the influence of myofascial restriction. Dr. Crawford is the founder of the Anchor Wellness Center & Anchor Wellness, Inc., an integrative health practice that specializes in physical therapy and pilates.

The body’s stress-response system is usually self-limiting. Once a perceived threat has passed, hormone levels return to normal. As adrenaline and cortisol levels drop, your heart rate and blood pressure return to baseline levels, and other systems resume their regular activities.
Thanks for your comment. While that may be true, that assumes that the threat ends. In those with chronic stress or pain, the threat persists.